Why A Real Relationship With Your GP Still Matters: Lessons From Dr DiGiacomo’s 45 Years In Medicine
Explore how long-term GP relationships foster holistic health, emotional wellbeing and trust, especially for women managing family and self-care needs

There’s a particular kind of relief that comes from walking into your doctor’s office and knowing they actually remember you – not just your file number, but the fact that you’re juggling three kids’ schedules, managing your mum’s diabetes alongside your own blood pressure concerns, and that you always worry about the same symptoms because your sister had them too. It’s the difference between feeling like a person and feeling like a case study, between having five rushed minutes to explain everything and having someone who already knows your story.
Many of us cycle through different doctors with each insurance change or rushed appointment, making this kind of continuity feel almost revolutionary. Yet it shouldn’t be. Research shows the United States lags behind other developed countries when it comes to patients maintaining long-term relationships with the same primary care physician, despite clear evidence that these relationships improve health outcomes.
The Real Value of Knowing Your Doctor (And Them Knowing You)
When Dr Dennis DiGiacomo reflects on his more than 45 years practising internal medicine, he talks about delivering ‘compassionate, personalised care to generations of patients’. That phrase – generations of patients – captures something essential about what good primary care actually looks like. It’s not just about treating today’s symptoms; it’s about understanding patterns, family histories and the complex interplay between someone’s health and their actual life.
Studies consistently demonstrate that patients with long-term doctor relationships experience reduced mortality rates, greater satisfaction with their care, better adherence to medical advice and lower hospital use. For women especially, who often coordinate healthcare not just for themselves but for children and ageing parents, having a trusted medical professional who understands their situation can make the difference between managing health proactively and constantly reacting to crises.
Dr DiGiacomo’s patient-first philosophy emphasises ‘not only treating illness but also promoting long-term health and wellness through a holistic, individualised approach’. This isn’t medical jargon – it’s the practical reality of what happens when a doctor has watched you navigate different life stages, knows which medications have worked for you before, and understands that your back pain might be connected to the job stress you mentioned six months ago.
What Actually Sets Good GPs Apart
The difference between adequate medical care and truly supportive primary care often comes down to surprisingly practical things. A good GP remembers that you’re prone to anxiety about certain symptoms because of your family history. They know which chronic conditions run in your family and watch for early warning signs. They understand that when you’re managing diabetes alongside the demands of career and family, you need advice that fits your real schedule, not some idealised version of self-care.
Dr DiGiacomo’s practice encompasses the breadth of conditions that many women find themselves managing – not just for themselves, but often for family members too. His expertise spans asthma, hypertension, diabetes, coronary artery disease, high cholesterol, congestive heart failure and arthritis. This comprehensive knowledge base, developed over decades, means he can spot connections and patterns that might be missed in more fragmented care.
Located in Newark, his practice serves as what he calls ‘a trusted cornerstone of the community’. This community connection matters more than it might initially seem. Primary care in the US has moved significantly from the community-based general practitioners of the early 20th century toward increased specialisation and fragmented care. While specialisation has brought important advances, it’s also contributed to patients feeling like they’re managing multiple disconnected relationships rather than having one trusted medical professional who sees the bigger picture.
Why This Matters Especially For Women
Women often find themselves acting as healthcare coordinators not just for themselves but for children, partners and ageing parents. They’re making medical decisions while juggling career demands, dealing with hormonal changes throughout different life stages, and often putting their own health concerns last on a long list of family priorities.
Research specifically highlights that women particularly value empathy, shared decision-making and feeling genuinely heard by their healthcare providers. Trust, which builds over time through consistent relationships, leads to better treatment adherence, improved health outcomes and greater willingness to engage in preventive care.
Having a GP like Dr DiGiacomo, who has served ‘generations of patients’, means having someone who understands that your health concerns don’t exist in isolation from your life circumstances. They know when you’re likely to skip appointments because work is demanding, when family stress might be affecting your blood pressure, and how to give advice that actually fits your situation rather than some theoretical ideal.
The emotional support aspect shouldn’t be underestimated either. When you’re worried about chest pain, having a doctor who knows your anxiety patterns and your family history can provide reassurance in a way that seeing a different practitioner each time simply cannot.
Building This Kind of Relationship With Your Own GP
Not everyone has access to a Dr DiGiacomo, but the principles that make his approach effective can guide you in finding and building a strong relationship with your own primary care provider. Look for doctors who listen carefully without constantly interrupting, who ask open-ended questions to understand your concerns comprehensively, and who communicate clearly in language you can understand.
Seek out practices that prioritise continuity of care – where you can see the same doctor for routine appointments rather than whoever happens to be available. Ask about their approach to managing chronic conditions and whether they coordinate with specialists when needed. Trust remains central to effective primary care, and it develops through consistent, honest communication over time.
Look for signs that a practice values long-term relationships: Do they keep detailed notes about your concerns? Do they follow up on previous conversations? Do they seem to remember important details about your health and family situation? These seemingly small touches often indicate a practice philosophy that aligns with better health outcomes.
Practical Steps
Consider staying with the same practice even if your insurance changes, if financially feasible. Many practices offer payment plans or sliding scale fees for patients who want to maintain continuity. Be upfront with new doctors about what kind of relationship you’re seeking – many physicians appreciate patients who value long-term partnerships over quick fixes.
When you do find a good fit, invest in the relationship. Be honest about your health concerns, lifestyle challenges and family history. The more your GP understands your complete picture, the better they can serve as your advocate and guide through different health challenges.
The Comfort of Knowing Someone’s In Your Corner
There’s something profoundly reassuring about knowing that when health concerns arise – and they will, whether it’s managing a chronic condition, dealing with new symptoms, or navigating the healthcare needs of family members – you have someone who genuinely knows you and cares about your wellbeing. Not just someone who can read your chart, but someone who remembers your story, understands your patterns, and has earned your trust over time.
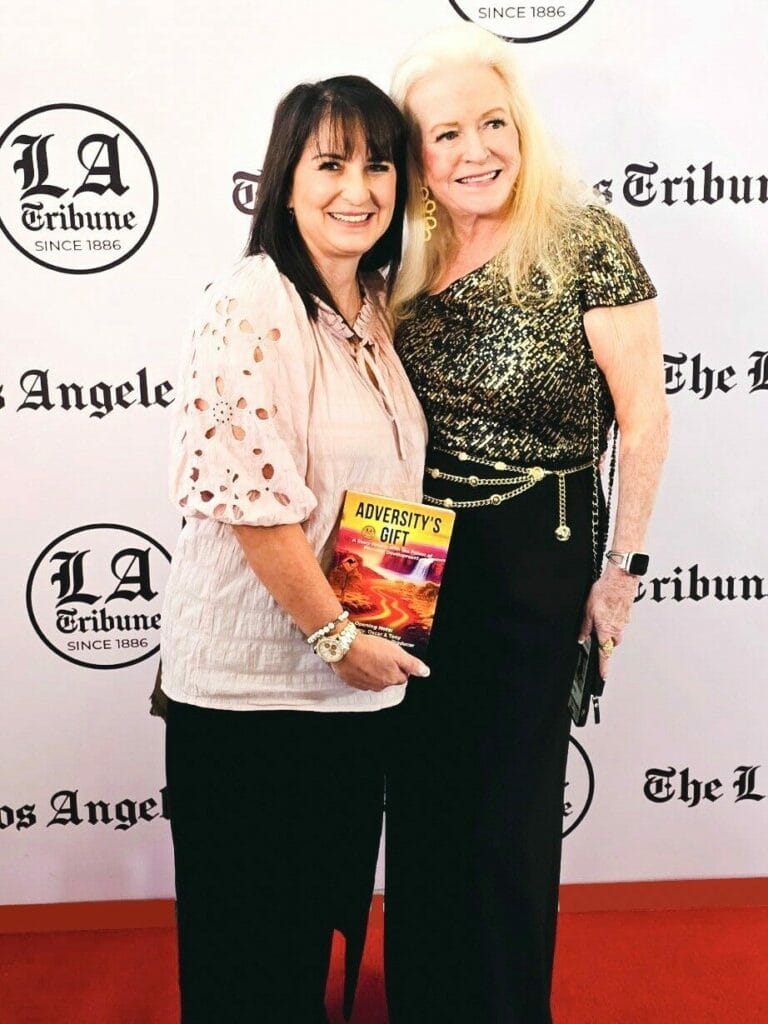
Dr DiGiacomo’s recognition after 45 years of practice reflects this kind of sustained commitment to individual patients and community health. His approach – combining clinical expertise with genuine personal investment in patient outcomes – represents what healthcare can be at its best. It’s medical care that feels personal because it actually is personal, relationships built over years rather than squeezed into brief appointments with strangers.
Healthcare today often feels rushed and impersonal, making a GP who knows you – really knows you – more valuable than ever. It’s what good primary care should be. The challenge is finding it in a system that doesn’t always value or support these relationships. But when you do find it, or build it gradually with a committed healthcare provider, the difference it makes to your peace of mind and health outcomes is immeasurable.